You are here
Vaccine Requirements Predate the COVID-19 Pandemic by More than a Century

A woman in Italy is vaccinated before travel in 1951. (Photo: International Organization for Migration)
The COVID-19 pandemic and restrictions to fight transmission of the virus have shined a spotlight on the linkages between border control and infectious disease management. In particular, development of vaccines to safeguard against the disease have paved the way for government mandates that most travelers prove prior immunization before entering Australia, the United States, European and Asian countries, and others.
Although the scale and disruption of the pandemic is in several ways unprecedented, these kinds of vaccine requirements are not. Contrary to what some recent public criticism might suggest, governments have periodically imposed similar conditions on travelers for more than a century, starting with smallpox in the 19th century. Early vaccine certification requirements predated the existence of government-issued passports. In fact, the first such requirements did not require a physical “vaccine passport” at all, but instead could be certified by a traveler’s smallpox scars or the marks from a vaccination.
Since the 1920s, vaccine certification has been an internationally recommended approach to manage the spread of infectious disease. Historically, travelers without certifications were vaccinated on the spot, underwent quarantine, or returned to their point of departure. These certification requirements have generally not been very controversial. Even immediately before the COVID-19 outbreak, 121 countries required some travelers to prove they had been vaccinated against yellow fever, and many also had mandates for polio or meningococcal meningitis (see Figure 1). Bangladesh also requires returning Hajj pilgrims to provide proof of being inoculated against influenza.
Figure 1. Countries Requiring Proof of Vaccination of Select Diseases Before Entry, 2021
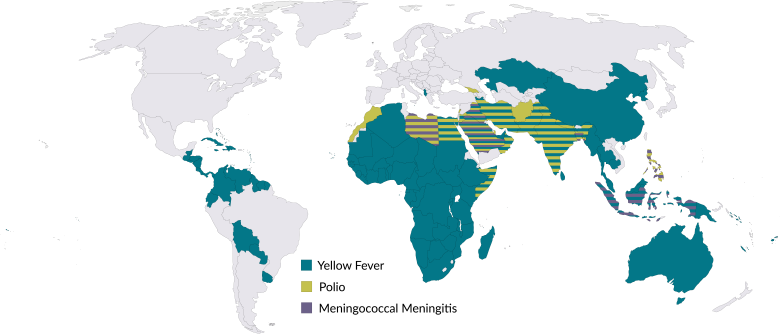
Note: Figure shows countries with any vaccine requirements for new arrivals; only 18 countries require all arrivals to be vaccinated against yellow fever. Data do not reflect national requirements for vaccination against COVID-19.
Source: Authors’ analysis of World Health Organization (WHO), International Travel and Health—12 May 2021 (Geneva: WHO, 2021), available online.
The history of these documents includes some episodes to be avoided and others which might have productive implications for the current moment. But rather than viewing today’s vaccination certifications (which can be physical or digital) as novel developments, it is more useful to understand them within the context of the slowly growing bureaucratic administration of health services over the last two centuries. As the world continues working out how to live with COVID-19 and more fully resume international travel, verifying vaccination promises to be one of the more vexing problems for the medium and longer terms. The world lacks a uniform system for registering and proving vaccination, but history shows that this too is not a new challenge. This article reviews the history of vaccine requirements as a condition for international travel in the 19th and 20th centuries, beginning with requirements related to smallpox and including the development of the World Health Organization (WHO) system for tracking vaccination status.
What Is a 'Vaccine Passport’?
The term “vaccine passport” has been used to describe an array of methods for certifying individuals have been inoculated against specific diseases. These can include paper cards, smartphone apps, and, historically, even physical scars. The World Health Organization’s Carte Jaune (Yellow Card) is the current standard vaccine certification document worldwide, particularly for international travel, but there is a wide array of methods for proving vaccination.
Certificates have proliferated particularly amid the COVID-19 outbreak, when many governments and private businesses have demanded that individuals prove they have been vaccinated before attending concerts, sporting events, and other public gatherings. These certifications have been colloquially referred to as “vaccine passports,” although their primary goal is not to facilitate international movement.
Smallpox and Early Vaccine Requirements
States have long coupled vaccinations with the movement of people across borders. Edward Jenner's technique of using cowpox vaccination to prevent smallpox, published in 1798, moved quickly from the farmlands of Gloucestershire, England across the British Empire, at first literally on children’s bodies through the “arm-to-arm” process involving orphans acting as live carriers of the vaccine aboard ships, which was carefully documented. Smallpox was a devastating disease that killed hundreds of millions of people before its eradication in the late 20th century, and halting its spread had long been a top concern for public-health professionals.
In British India, the practical application of vaccinations as a sanitary principle was clear to colonial administrators, who were concerned with managing large populations of laborers moving around the Indian subcontinent and mitigating the spread of infections into rural areas. After a few logistical hurdles, colonial powers in 1827 established the Bombay system of smallpox vaccination, which involved a tiered system of European superintendents who oversaw locally recruited vaccinators. In 1877, the Bombay Vaccination Act explicitly prohibited unvaccinated people or people who had been inoculated for less than 40 days from entering certain local areas. Included in the law was a provision allowing designated medical practitioners and local government officials to write certificates stating that an individual was “no longer likely to produce smallpox by contact or near approach.”
Bodily Scars as Evidence of Immunity
At first, however, these types of government-issued certificates were rare. Smallpox was a highly visible disease, usually leaving its survivors permanently pock-marked. But the lifelong scars, often on individuals’ faces, had occasionally unexpected benefits: signaling protection from recurring disease, even at a time before doctors fully understood the processes of immunity. In this manner, smallpox scars could function as a certification of their own, assuring other members of the public that the individual could not spread the disease. In early 20th century Canada, for example, clearly identifiable old smallpox scars served as an assurance at seaports that the disease itself was not being introduced through maritime traffic.
For more people in the 19th and early 20th centuries, however, having a single mark—the scar produced by receiving the cowpox-laden vaccine—was the more authoritative verification. Displaying just one scar, usually on the left upper arm, was the earliest widely accepted proof of vaccination. With growing global confidence in the protective power of vaccines towards the turn of the century, that mark itself identified the vaccination status of an individual, and sometimes enabled them to move over domestic, intercolonial, and international borders.
In 1881, for example, there was an epidemic of smallpox in Sydney. Just as during the months following the outbreak of COVID-19, travel between Australia’s states was strongly policed, trains were commonly stopped, and authorities inspected passengers for risks to public health. Only travelers with a visible vaccination scar were permitted entry into the neighboring “clean” colony of Victoria. These restrictions were later eased after approximately six months. Three decades later, in response to a 1913 outbreak, a similar system was instituted, this time with a tighter a radius of 15 miles from the Sydney General Post Office. Restrictions went only one way: unvaccinated inhabitants of metropolitan Sydney were unable to travel outside this quarantine perimeter for 145 days, but there were no such requirements for those wishing to enter Sydney or the state of New South Wales from elsewhere.
In other instances, the smallpox vaccination scar allowed travelers to cross international borders. At a time when significant long-distance travel occurred via sea, this meant inspection at ports of departure or arrival. In countries where smallpox was not endemic, the vaccine scar became increasingly a requirement for new arrivals, especially immigrants. For some governments, it was also a condition of embarkation, especially if smallpox was present at the port of departure. Migrants travelling from England to Canada, for example, needed to show evidence of “having been vaccinated, or of already having had smallpox,” according to the quarantine regulations. In general, most travelers without proof of vaccination were refused embarkation or entry, and since shipping companies themselves were often liable for the cost of a traveler’s return to their point of departure, inspections by ships’ doctors were thorough. First-class passengers, however, were more likely to be able to evade inspection.
The Rise of Paper Vaccine Certificates
Over time, jurisdictions demanded more conventional paper certification of smallpox vaccination. In early 20th century Canada, a medical Inspection Card listing one’s vaccine history needed to be signed, kept for three years, and presented to government officials when required. In Australia around the same time, Personal Detail Cards recorded an individual’s vaccine history in greater detail than a scar ever could, including by listing where, when, and by whom the vaccine was administered, with what specific vaccine, and how the individual reacted (in terms of size, color, and discharge at the vaccine site).
Such paper certification of smallpox vaccination served as an early identification document at a time when passports themselves were unusual. Most governments did not yet require what have since become conventional passports to prove one’s identity for international travel, which were mostly developed during the 20th century.
These types of documents evolved as part of a broader trend. Vaccination certificates, also commonly referred to as health certificates, accompanied the normalization of other kinds of certification in modern states, such as for birth, death, and marriage. Carrying documentary verification of one’s vaccination history became increasingly normalized. In countries with growing public health bureaucracies, doctors would typically document smallpox vaccination and revaccination, compile these episodes into government data, and use these statistics to calculate the proportion of the population that was covered. This was a means of tracking herd immunity, which is a term in recent years that has become increasingly familiar. In places experimenting with compulsory vaccination programs, such as the United Kingdom around the time of the 1867 Imperial Vaccination Act, authorities provided parents with certificate duplicates.
Polio, Yellow Fever, Cholera, and Meningococcal Meningitis
Polio is another dreaded disease that can lead to permanent paralysis. A successful polio vaccine was developed in 1954, but it was not until 1988 that WHO initiated a worldwide eradication campaign relying on national vaccination efforts. This campaign was responsible for the drastic reduction of polio over subsequent decades, however the disease has not been totally eliminated worldwide. Nineteen countries continue to require certain travelers produce proof of vaccination before entry, mostly those arriving from places where polio is endemic.
After the eradication of smallpox and control of polio, most travel vaccine mandates have been designed to combat yellow fever. This disease, which is spread by mosquitoes and is endemic to tropical Africa and Central and South America, caused the deaths of so many U.S. soldiers in the 19th century that the U.S. military formed the Yellow Fever Commission in 1900 to investigate the disease and ways to control it. It was not until 1936 that the first vaccine against yellow fever was developed by Max Theiler, and later was used widely in tropical Africa through the 1960s, where the eradication of the disease seemed possible. However, international complacency, insufficient vaccine supply, and increased air travel have all lead to epidemic yellow fever outbreaks in the last 30 years.
According to WHO, 121 countries currently require proof of valid yellow fever vaccination before entry. This requirement applies predominantly to those arriving from or transiting through countries that are deemed to be at risk of the disease, but 18 countries—primarily in Central and West Africa—require all travelers to provide vaccination documentation regardless of their origin. WHO also separately recommends yellow fever vaccination when travelling to 40 countries, not all of which require the jab for all travelers.
The disease has been tenacious. In 2016, a yellow fever outbreak in Angola spread as far as China. In response, WHO launched the Eliminate Yellow Fever Epidemics (EYE) global strategy, a central tenet of which is targeting travelers and improving adherence to entry and departure vaccination requirements.
Other vaccines that have historically been a part of some travel restrictions are for cholera and meningococcal meningitis. Cholera vaccines are no longer required as a travel requirement, although can be recommended for travelers to areas with active cholera transmission. Because cholera spreads through contaminated food and water, improvements to infrastructure and sanitation over the second half of the 20th century rendered vaccination certificates for this disease less pressing.
However, the meningococcal vaccine, first developed in the 1970s, is still required for some travelers in seven countries and is also recommended to those travelling to sub-Saharan Africa’s “meningitis belt,” which runs from Senegal to Ethiopia. The disease has a high morbidity rate, but scholars have found that more education is required for travelers to improve vaccine uptake.
Vaccine Certificates: An Inconsistent System
Before modern electronic registration and QR codes, what did health certificates look like? The documents contained three basic elements: the identity of the certificate holder, the date on which they were vaccinated, and the signature or stamp of the authority. While these features may seem common sense, the path to regulating such documents was rarely straightforward. Changes were constantly made in response to fraudulent activities and evolving exit requirements.
These days, most COVID-19 vaccination certificates for international travel are used as a complement to one’s passport, reinforcing the notion that disease protection is a component of the broader system of migration and travel surveillance. This arrangement also means that passport photographs and other data can be used to verify the vaccinated person’s identity. But as previously mentioned, official passports were not compulsory documents for travel in the early 20th century, so travelers were previously advised to have photos affixed to vaccination certificates themselves. And even still, problems persist; during Angola’s 2016 yellow fever outbreak, migrant workers used counterfeit vaccination cards to cross land borders and unwittingly spread the disease.
A Mosaic of Rules and Requirements
Historically, governments instituted timeframes that stipulated how long travelers had between receiving a vaccination and entering the country, but these regulations were not uniform. For cholera in the 1930s, for example, most ports mandating proof of vaccination required travelers to have received their inoculations between six days and six months before arrival, as recommended in the International Sanitary Convention of 1926, or else they faced quarantine and, at times, blocked passage. The quasi-colonial concession of Shanghai, however, barred travelers who got their shots more than four months before entry (there was no minimum time frame). Quarantine authorities in the Philippines, meanwhile, did not recognize inoculations more than three months old, unless the individual had been vaccinated multiple times: four and a half months from the first dose for those with two vaccinations, and six months for individuals with three doses. In response to an outbreak, the United States in 1947 required cholera vaccination cards for travelers who had previously passed through Egypt, India, or Pakistan; two shots were required, with not less than six days or more than ten between the two doses, and travelers without proof had to undergo five days of quarantine.
Issuing authorities also varied. Some of the earliest vaccination certificates were authenticated by a doctor’s signature, but at times these jabs were administered by an apprentice. Stories were common of doctors facing criminal charges for issuing certificates for unsuccessful smallpox vaccinations, and frequently the apprentice became the scapegoat.
By the turn of the 20th century in places where public health bureaucracies were established, stamps from health departments were increasingly a required component of the certificate. In places such as Sydney during the 1913 smallpox outbreak, these stamps replaced doctors’ signatures as the seal of approval. In the 1940s in Hong Kong, the exposure of a business racket trading in forged vaccine certificates led authorities to strip doctors of their ability to certify smallpox and cholera vaccinations for travel. Instead, the Port Authority started registering and cross-referencing doctors’ signatures, until doctors were permitted to resume certifications in 1948. The process of medical and public health bureaucratization and administration was thus increasingly normalized across the 20th century.
Intermittent Requirements at Different Destinations
Outbreaks of diseases such as smallpox and cholera were episodic during the first half of the 20th century, so requiring proof of vaccination for travel was similarly enforced intermittently by different ports of entry, depending on disease spread. Take the case of Hong Kong in the 1920s, then a Crown colony of Britain and a site of significant health surveillance due to its status as an entrepôt. When an outbreak occurred there, officials in airports and seaports across Asia, Egypt, and the United States would impose quarantines and vaccination inspections on vessels arriving from the colony. By the 1930s, a port’s simple declaration that a single arrival from Hong Kong was infected with smallpox or cholera would automatically trigger the requirement for all travelers on the route to supply a valid vaccination certificate.
At times, the inspection of health certificates only applied to certain classes of passengers. For example, in 1937 the standing rule demanded all passengers from Hong Kong embarking in the Philippines prove they had been vaccinated against cholera, or else they were prohibited from leaving or forced to undergo vaccination and then quarantine at the landing port. But by the following September, first- and second-class cabin passengers were exempt from inspections; only passengers in steerage class, the lowest level of ship travel, were required to provide a valid vaccination certificate stamped by a Hong Kong government medical officer or port health officer. Other ports, including some in the United States, also applied this double standard to arrivals from Hong Kong. The colony itself required migrant workers to hold a vaccine certificate should they want to leave for mainland China and re-enter. Although never explicitly stated as such, the decision reflected the prevalent and misplaced association that the poor were a carrier of disease, particularly cholera. Vaccine certificates, however, were not always free, so the burden of proof was heavier and costlier for those who could least afford it.
Towards an International System in the 20th Century
The 1926 International Sanitary Convention was the first multilateral protocol that recommended using vaccines as a condition of cross-border movement, which it did for cholera. Because, it noted, vaccination was “a method of proved efficacy in staying cholera epidemics,” all sanitary administrations “in the largest measure possible and as often as practicable… [should] grant certain advantages as regards restrictive measures to persons who have elected to be vaccinated.” Forty-four of the 66 signatory governments ratified the document. This marked the start of international cooperation to link vaccination to increasingly common international movement. With the wider availability of air travel, the International Sanitary Convention for Aerial Navigation of 1933 mirrored the 1926 convention except that it was designed to include airports. This was also the first international treaty to suggest standardized international certificates of vaccination. By 1944, templates for such internationally recognized certificates existed for cholera, smallpox, typhus, and yellow fever.
Not every traveler was required to prove vaccination under this regime, only those travelling from a port with a declared outbreak or where a disease was considered endemic. What became increasingly crucial, then, was the international commitment to report and share disease incidence, which had been discussed and attempted to some degree since the 1850s. Local medical inspection and, often, quarantine of potentially infected travelers was also important.
When WHO was established in 1948, a century of overlapping and inconsistent international health regulations had created a messy landscape. The new UN agency sought to streamline processes and in the 1950s issued the Carte Jaune (or Yellow Card) which became the standard vaccination certification document worldwide. These booklets have provided a means for physicians to systematically record details of a vaccination, including the manufacturer and batch number, as well as personal details that replicate those displayed in an individual’s passport. Although the Carte Jaune is often associated with yellow fever, it was not explicitly issued for this disease. It remains in existence as the internationally accepted certificate demonstrating vaccination status.
Migration and Infectious Disease Management: Long Intertwined
Although the prospect of a “vaccination passport” has heightened opposition to sensible pandemic management in some quarters, the use of some health checks as a component of migration regulation has been standard for decades. Aside from vaccines, almost every migration statute across the world contains a clause enabling border officials to check some health documentation in certain cases, such as certification of clear chest X-rays for tuberculosis. In other words, migration and the management of infectious disease—including the certification of vaccination—have been intertwined for more than a century. As this long global history shows, recent requirements for certifications around COVID-19 vaccination are anything but exceptional.
Sources
Bashford, Alison. 2003. Imperial Hygiene: A Critical History of Colonialism, Nationalism and Public Health. London: Springer.
Bhattacharya, Sanjoy, Mark Harrison, and Michael Worboys. 2005. Fractured States: Smallpox, Public Health and Vaccination Policy in British India 1800-1947. New Delhi: Orient Longman.
Commonwealth of Australia. 1913. Provisional Regulations under the Quarantine Act 1908-1912.
Fidler, David P. 2005. From International Sanitary Conventions to Global Health Security: The New International Health Regulations. Chinese Journal of International Law 4 (2): 325-92. Available online.
Frierson, J. Gordon. 2010. The Yellow Fever Vaccine: A History. Yale Journal of Biology and Medicine 83 (2): 77-85. Available online.
Goodman, Anna L., Cristina Masuet-Aumatell, Jay Halbert, and Jane N. Zuckerman. 2014. Awareness of Meningococcal Disease among Travelers from the United Kingdom to the Meningitis Belt in Africa. The American Journal of Tropical Medicine and Hygiene 91 (2): 281. Available online.
Hong Kong Government Gazette. 1938-1941. Hong Kong: Noronha & Co. Available online.
Howard-Jones, Norman. 1975. The Scientific Background of the International Sanitary Conferences 1951-1938. Geneva: World Health Organization. Available online.
United Nations. 1944. International Sanitary Convention for Aerial Navigation, 1944 (with Annexes), Modifying the Convention for Aerial Navigation of 12 April, 1933. Available online.
---. 1944. International Sanitary Convention of 1944, Modifying Convention of 21 June 21, 1926.
South China Morning Post. 1939. Port Requirements. 1939. South China Morning Post, August 30, 1939.
---. 1940. Passengers to Malaya: Regulations for Cholera and Small-Pox Certificates. South China Morning Post, February 22, 1940.
---. 1941. Philippines Rules: Cholera Inoculation Insisted Upon. South China Morning Post, June 14, 1941.
Plotkin, Stanley A., Walter A. Orenstein, and Paul A. Offit. 2013. Vaccines: Sixth Edition. Philadelphia: Elsevier.
Riedel, Stefan. 2005. Edward Jenner and the History of Smallpox and Vaccination. Baylor University Medical Center Proceedings 18 (1): 21-25. Available online.
Sealey, Anne. 2011. Globalizing the 1926 International Sanitary Convention. Journal of Global History 6 (3): 431-55.
Argus. 1913. Small-Pox in Sydney. Argus, July 5, 1913.
Trişcaş, Floarea Elena. 2013. Epidemics of Smallpox and the Introduction of Vaccines in the Bistriţa Region (XVIII-XIX Centuries). Procedia - Social and Behavioral Sciences 92 (10): 947-52.
World Health Organization (WHO). 2012. International Travel and Health: Situation as on 1 January 2012. Geneva: WHO. Available online.
---. 2016. Global Strategy to Eliminate Yellow Fever Epidemics (EYE): Document for SAGE – 26 September 2016. Geneva: WHO.
---. 2021. International Travel and Health—12 May 2021. Geneva: WHO. Available online.


